Birth at 26 weeks gestation is a topic that elicits a spectrum of emotions, underscored by both hope and trepidation. At this juncture, infants are classified as extremely preterm. The medical landscape surrounding their survival is being profoundly redefined by advances in neonatal care. This article delves deeply into the survival rates associated with 26-week-old fetuses, examines the factors influencing these rates, and explores the implications for medical science and families alike.
The Biological Reality of Prematurity
At 26 weeks of gestation, a fetus has reached a critical developmental milestone, yet remains physiologically fragile. The lungs, while increasingly functional, are still immature. The cerebral cortex, crucial for cognitive development, continues to undergo formation. Thus, understanding the precarious balance of survival hinges on grasping these biological nuances. Survival statistics reveal a harrowing dichotomy; while the survival rates have significantly improved, they are unequalled by the challenges that lie ahead.
Survival Statistics: A Closer Look
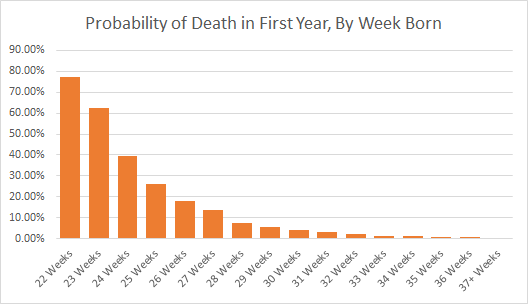
Research demonstrates that survival rates for infants born at 26 weeks have improved dramatically over the past few decades, with current estimates hovering between 80-90% in well-resourced medical facilities. This figure, however, belies the complexities of preterm birth, which encompasses not merely the act of survival but also the myriad complications that can arise postnatally. These complications, often categorized under the umbrella of prematurity-related medical conditions, can impose substantial burdens on the infant’s long-term health.
The Role of Medical Interventions
The landscape of neonatal care continues to evolve, characterized by significant advancements in medical technology and interventions. Innovations such as continuous positive airway pressure (CPAP), surfactant therapy, and meticulous monitoring of vital signs have transformed the care paradigms for these vulnerable neonates. CPAP, for instance, aids in maintaining adequate oxygenation, thereby counteracting the precursors of respiratory distress syndrome. Surfactant replacement therapy enhances lung function, ultimately improving the likelihood of survival.
Furthermore, the emergence of neonatology as a specialized field has catalyzed the development of tailored approaches to care. The integration of multidisciplinary teams, including pediatricians, respiratory therapists, and lactation consultants, creates a holistic approach to infant care, fostering not just survival but thriving.
Factors Influencing Survival Rates
Several extrinsic and intrinsic factors converge to affect survival rates at 26 weeks. Maternal health status, for example, plays a pivotal role. Conditions such as hypertension, diabetes, or infections can compromise fetal health, thereby adversely affecting neonatal outcomes. Access to prenatal care is paramount; early interventions can rectify complications in the intrauterine environment, effectively improving prognoses.
Moreover, gestational factors, including twins or higher-order multiples, pose additional risks necessitating a nuanced understanding of prenatal development. The interplay of the number of fetuses and their gestational age can exacerbate the challenges, leading to a cascade of medical interventions.
Postnatal Complications: The Hidden Dangers
Survivability is far from a linear process. Even with the current statistics suggesting a favorable outcome, the reality is steeped in potential challenges. Premature infants are at increased risk for several lifelong health issues, which can range from mild to severe. Conditions such as bronchopulmonary dysplasia (BPD), retinopathy of prematurity (ROP), and neurodevelopmental disorders may arise, often necessitating intensive follow-up care. The implications for family dynamics, educational needs, and future health are significant and serve as reminders of the complexities of premature birth.
Long-Term Outcomes: An Uncertain Future
The quest for understanding doesn’t cease once an infant leaves the neonatal unit. Studies have indicated that while many survive, they may experience challenges related to cognitive and physical development. Children born at 26 weeks may face difficulties in motor skills, learning disabilities, and social-emotional challenges. While some overcome these hurdles, others may require ongoing intervention and support throughout their lives, establishing an intricate relationship between prematurity and lifelong health trajectories.
Ethical Considerations in Care
The medical community continues to grapple with ethical dilemmas surrounding the care of extremely preterm infants. Decisions regarding the extent of medical intervention at 26 weeks raise challenging questions about quality of life, parental values, and societal perspectives on disability and health. The continuum of care necessitates framing clinical choices within the context of informed consent and ethical principles, fostering a partnership between families and healthcare providers.
The Evolving Role of Research and Advocacy
In an era where medical science is continually progressing, research plays an indispensable role in shaping best practices. Clinical trials, observational studies, and evidence-based protocols are crucial in refining approaches to care, ultimately translating into improved outcomes for infants born at 26 weeks. Advocacy groups have amplified their efforts to raise awareness and disseminate critical information regarding the realities of prematurity, cultivating a better-informed public and healthcare community.
The Future of Neonatal Care
The discussion surrounding the survival of infants born at 26 weeks is laden with both tension and hope. As medical science continues to advance, the landscape will likely undergo further transformation, with potential repercussions for how neonates are cared for in the future. The continued exploration of genetic interventions, personalized medicine, and innovative technologies holds promise for optimizing outcomes and mitigating the long-term effects of prematurity.
In conclusion, while the survival rates for 26-week-olds are indeed encouraging, the multidimensional nature of their care and the implications of their birth must not be overlooked. The intersection of empathy, ethics, and science will remain pivotal as society navigates the jurisdictions of hope and reality, ultimately reshaping the narrative of prematurity in the years to come.