The continent of Africa is vast and replete with a myriad of cultural landscapes, diverse ecosystems, and complex socio-economic contexts. Concomitant with this diversity, however, are profoundly variable life expectancies among its populace. Understanding the average death age in Africa necessitates a nuanced exploration of health systems, cultural attitudes towards life and death, as well as the socio-economic factors that converge to shape mortality rates. This exploration will highlight a journey through a continent laden with challenges but also brimming with hope.
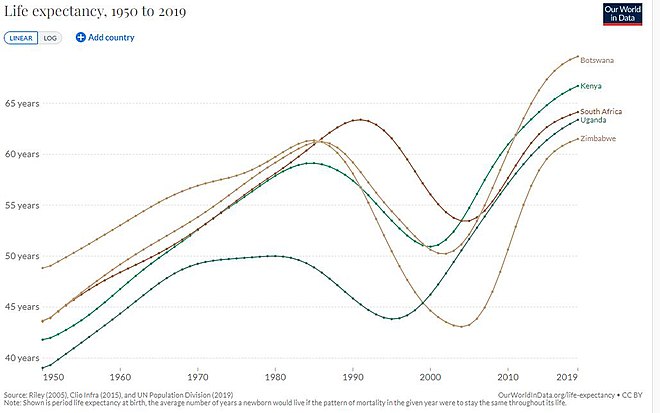
Life expectancy is often utilized as a primary indicator of a nation’s health and quality of life. In many African countries, this figure lags behind global averages, primarily due to a confluence of factors including infectious diseases, malnutrition, and, increasingly, non-communicable diseases. Sub-Saharan Africa, in particular, faces significant health challenges that contribute to lower average death ages. Countries such as Nigeria, Angola, and the Democratic Republic of Congo exhibit some of the lowest life expectancies globally, where endemic diseases, coupled with limited access to healthcare, culminate in high mortality rates, often skewing the average death age towards earlier years.
One cannot discuss health in Africa without acknowledging the stigma and systemic shortcomings surrounding healthcare access. The inequity in healthcare systems reveals stark disparities based on geographical, socio-economic, and cultural divides. Rural communities often grapple with inadequate medical facilities, a lack of trained healthcare personnel, and insufficient infrastructure. The urban-rural dichotomy is stark; metropolitan areas may sport modern healthcare facilities yet still reflect the nation’s broader health challenges. This observation engenders a cultural relativism perspective, urging stakeholders to appreciate local customs and healthcare beliefs, rather than imposing external standards of health and wellbeing.
Alongside cultural considerations, African nations are actively engaging in the promise of resilience and revitalization within their healthcare systems. Initiatives aimed at combating diseases such as HIV/AIDS, tuberculosis, and malaria have seen substantively increased investment in public health. The World Health Organization and numerous NGOs have played pivotal roles in enhancing healthcare access, education, and preventive measures across the continent. Despite the existing challenges, countries such as Rwanda have achieved notable successes and have become models for public health reform in the region.
The health landscape of Africa is intricately interwoven with cultural perceptions about illness, mortality, and wellness. Traditional medicine systems remain prevalent, often coexisting with modern healthcare practices. In various communities, local healers are respected figures who provide not only medical treatment but also social and spiritual support. This duality enhances resilience among populations facing health adversities. The intertwining of tradition and modernity in health reflects a broader anthropological narrative: the need to respect and validate local beliefs in the pursuit of health improvement.
As a result of the intricate tapestry of cultural beliefs and systemic healthcare challenges, the average death age in Africa embodies both a critical lens through which to understand health disparities and a focus point for amelioration efforts. The juxtaposition of despair and hope threads through the narrative of health in Africa. The continent is not solely defined by its struggles; rather, it also showcases remarkable advancements in technology, public health policy, and community health initiatives.
Moreover, education plays a pivotal role in shifting health outcomes. Increased investment in education, particularly for women, has been shown to correlate with improved health metrics. Educated women are more likely to access healthcare resources, engage in preventive measures, and advocate for their own and their families’ health. Consequently, elevated educational attainment has the potential to engender multi-generational transformations in the average age of death across Africa.
Nevertheless, the specter of chronic illness looms larger as lifestyles shift and urbanization accelerates. As more individuals migrate to urban areas, they often adopt sedentary lifestyles and increased consumption of processed foods, exacerbating the prevalence of non-communicable diseases such as diabetes and hypertension. This epidemiological transition raises pertinent questions regarding future mortality trends and the experiences of aging populations, highlighting the intersection of cultural adaptation and health outcomes.
In contemplating the future, one must consider the untapped potential that exists within Africa’s vibrant communities. Collaborative efforts among governments, non-profit organizations, and local communities hold promise for innovation and tailored approaches to health improvement. Future strategies must advocate for holistic health solutions that not only address immediate medical needs but also encompass education, economic improvement, and cultural respect.
Ultimately, the narrative surrounding average death age in Africa encapsulates a complex interplay of health, culture, and socio-economics that demands a comprehensive and empathetic approach. It is clear that while significant challenges remain, the resilience of African nations, bolstered by a rich tapestry of cultural practices and emerging health initiatives, points to a future where health and hope may harmonize. As we navigate this multifaceted terrain, a shift in perspective is imperative—one that acknowledges the unique cultural intricacies of African healthcare and embraces the potential for transformative change that resides within its communities.